How to start a functional medicine practice is a journey that begins with understanding a revolutionary approach to healthcare. This guide delves into the core principles of functional medicine, contrasting it with conventional methods and exploring the foundational philosophy that guides practitioners. You will discover the typical patient journey, gaining insight into how this patient-centered model transforms health outcomes.
We will meticulously navigate the essential steps, from establishing a robust legal and regulatory framework to developing a comprehensive business plan. The operational framework, service offerings, team building, and marketing strategies will be explored in detail, ensuring you have a clear roadmap. Furthermore, we will cover patient care protocols, financial management, and the crucial aspects of continuous improvement and growth, equipping you with the knowledge to build a thriving practice.
Understanding the Functional Medicine Model

Embarking on the journey to establish a functional medicine practice is akin to cultivating a garden of holistic well-being. It requires a deep understanding of the soil, the seeds, and the intricate dance of life that allows for true flourishing. This model isn’t merely a different approach to healthcare; it’s a paradigm shift that honors the interconnectedness of our physical, mental, and spiritual selves.The functional medicine model is a systems biology-based approach that focuses on identifying and addressing the root causes of disease.
Rather than simply suppressing symptoms, it seeks to understand the complex interactions among genetic, environmental, and lifestyle factors that can influence chronic illness and health. This approach views the body as an integrated whole, recognizing that imbalances in one area can manifest as symptoms in another.
Core Principles of Functional Medicine
The foundational tenets of functional medicine are rooted in a profound respect for the individual’s unique biological makeup and life experience. These principles guide practitioners in uncovering the underlying causes of health concerns and empowering patients to reclaim their vitality.
- Biochemical Individuality: Each person possesses a unique genetic blueprint and environmental exposure history, leading to distinct physiological responses. This means that what works for one individual may not be optimal for another, necessitating personalized interventions.
- The Patient as a Whole: Functional medicine views health and illness as existing on a continuum. It emphasizes the interconnectedness of all body systems and the influence of lifestyle, environment, and emotional well-being on physical health.
- Root Cause Analysis: Instead of merely managing symptoms, functional medicine practitioners delve deep to uncover the fundamental origins of disease. This often involves exploring genetic predispositions, environmental toxins, dietary patterns, stress levels, and sleep quality.
- Healing is an Active Process: The patient is an active participant in their healing journey, not a passive recipient of care. Functional medicine empowers individuals with knowledge and tools to make sustainable lifestyle changes that promote lasting health.
- Physiological Imbalances: Chronic illness is often the result of underlying physiological imbalances that have developed over time. Identifying and correcting these imbalances is key to restoring health and preventing future disease.
Differences Between Conventional and Functional Medicine Approaches
The divergence between conventional and functional medicine lies in their fundamental philosophy and methodology. While conventional medicine often excels at acute care and symptom management, functional medicine shines in its ability to address the complexities of chronic disease and promote optimal wellness.
Conventional medicine typically operates on a disease-centered model, where the focus is on diagnosing and treating specific illnesses by targeting symptoms with pharmaceuticals or surgery. This approach is vital for emergencies and acute conditions but can sometimes fall short in addressing the multifaceted origins of chronic diseases. In contrast, functional medicine adopts a patient-centered approach, viewing the individual as a complex system.
It seeks to understand the ‘why’ behind the symptoms by investigating the interplay of genetics, environment, and lifestyle. This allows for personalized interventions that address the root causes, aiming for a deeper and more sustainable return to health.
Consider the example of autoimmune disease. A conventional approach might involve prescribing immunosuppressants to manage the symptoms of inflammation. A functional medicine practitioner, however, would investigate potential triggers such as gut dysbiosis, food sensitivities, environmental toxins, or stress, and develop a personalized plan to address these root causes, potentially reducing the need for long-term immunosuppression.
Foundational Philosophy Guiding a Functional Medicine Practice
The guiding philosophy of functional medicine is one of deep reverence for the body’s innate capacity to heal and thrive. It is a philosophy that recognizes the profound wisdom of nature and the power of creating an internal environment conducive to optimal health.
“Health is not the absence of disease, but a state of vital, energetic, and creative living.”
This statement encapsulates the essence of the functional medicine ethos. It’s about more than just being symptom-free; it’s about cultivating a vibrant existence where one feels truly alive, capable, and engaged with the world. This philosophy encourages practitioners to move beyond a reactive stance to a proactive one, fostering a partnership with patients to build resilience and prevent illness before it takes hold.
It’s about understanding that the body is a self-regulating organism with an incredible ability to restore balance when given the right support.
Typical Patient Journey in a Functional Medicine Setting
The journey of a patient seeking functional medicine care is often one of discovery, empowerment, and transformation. It is a process designed to peel back the layers of complexity surrounding their health concerns and illuminate the path toward lasting well-being.
The initial phase typically involves an extensive initial consultation. This is not a rushed appointment but a deep dive into the patient’s history, encompassing their genetic predispositions, childhood experiences, diet, lifestyle, stress levels, sleep patterns, relationships, and emotional well-being. This comprehensive understanding allows the practitioner to see the patient as a whole person, not just a collection of symptoms.
Following this, a series of targeted assessments and laboratory tests are usually recommended. These might include advanced blood work, stool analysis, urine tests, or even genetic testing, depending on the individual’s needs. These tests go beyond standard screening to investigate the underlying physiological imbalances and identify specific root causes. For instance, a stool analysis might reveal imbalances in gut bacteria, which can be a significant contributor to various chronic health issues.
Based on the gathered information, a personalized, comprehensive treatment plan is developed. This plan is not a one-size-fits-all prescription but a dynamic roadmap tailored to the patient’s unique biochemistry and lifestyle. It often involves a multi-faceted approach, incorporating dietary changes, targeted nutritional supplements, stress management techniques, sleep optimization strategies, and, when necessary, the judicious use of conventional therapies. For example, a patient with chronic fatigue might receive a plan that includes specific dietary recommendations to support mitochondrial function, adaptogenic herbs to manage adrenal stress, and guidance on improving sleep hygiene.
The journey continues with ongoing follow-up appointments. These sessions are crucial for monitoring progress, making necessary adjustments to the treatment plan, and providing continued support and education. This iterative process ensures that the patient remains engaged and empowered throughout their healing journey, fostering sustainable health and a deeper connection with their own well-being.
Laying the Legal and Regulatory Foundation

Embarking on the journey of establishing a functional medicine practice is akin to tending a garden; it requires careful preparation of the soil before planting the seeds of healing. Just as the earth must be fertile and free from stones, your practice must be built upon a solid legal and regulatory framework. This foundational work ensures that your healing ministry can flourish with integrity, protecting both you and those you are called to serve.
It is a testament to your commitment to responsible and ethical practice, allowing your light to shine brightly without obstruction.The path forward involves understanding the essential structures that will support your practice’s growth and ensuring you are aligned with the governing principles that safeguard the sacred trust between practitioner and patient. These elements are not mere administrative hurdles; they are divine signposts guiding you toward a sustainable and impactful practice, reflecting the order and wisdom inherent in creation.
Business Structures
Choosing the right vessel for your practice is a crucial step, as it dictates how your business operates, how it is taxed, and the extent of your personal liability. Each structure offers a unique way to manifest your calling, and selecting the one that best aligns with your vision and your spirit is an act of stewardship. Consider these common pathways as you discern the best fit for your unique ministry of wellness.The primary business structures available to you are:
- Sole Proprietorship: This is the simplest form, where you and your practice are legally one. It is easy to set up but offers no protection for your personal assets from business debts or lawsuits. Think of it as a direct conduit of your energy and efforts, with no separation.
- Limited Liability Company (LLC): An LLC creates a legal distinction between you and your business. This separation shields your personal assets, offering a layer of protection. It provides flexibility in management and taxation, allowing for a balance between personal involvement and corporate structure.
- S-Corporation: An S-corp is a tax designation that can offer potential tax advantages for profitable businesses by allowing profits and losses to be passed through directly to the owners’ personal income without being subject to corporate tax rates. This structure can be beneficial as your practice grows and flourishes.
Licenses and Certifications
To offer your gifts and services, you must possess the recognized credentials that validate your expertise and your authority to practice. These licenses and certifications are like the blessings bestowed upon a craftsman, attesting to their skill and readiness to serve. Ensuring you have all the necessary approvals is a vital part of your ethical foundation, demonstrating your commitment to excellence and patient safety.A comprehensive checklist of essential licenses and certifications includes:
- Professional License: This is your fundamental credential, such as a medical license (MD, DO, ND), chiropractic license (DC), or licensed dietitian/nutritionist (RDN), depending on your primary scope of practice. It is the cornerstone of your ability to provide care.
- State and Local Business Licenses: These permits are required to operate a business within your specific geographical area. They signify your compliance with local regulations and your right to conduct commerce.
- Specialty Certifications: While not always legally mandated, certifications in functional medicine or related disciplines (e.g., Institute for Functional Medicine (IFM) certification) are crucial for demonstrating specialized knowledge and commitment to the functional medicine approach. These elevate your standing and attract those seeking your unique expertise.
- DEA Registration (if prescribing controlled substances): For practitioners authorized to prescribe controlled substances, this federal registration is a mandatory requirement.
Patient Privacy Compliance
The trust placed in you by your patients is a sacred bond, and safeguarding their personal health information is a profound ethical and legal obligation. Just as a priest guards the confidences shared in prayer, you must diligently protect the privacy of your patients’ sensitive data. Adherence to regulations like HIPAA is not merely a legal requirement; it is a spiritual commitment to honor and respect the vulnerability of those seeking your guidance.The Health Insurance Portability and Accountability Act (HIPAA) establishes national standards to protect individuals’ medical records and other protected health information (PHI).
Key compliance requirements include:
- Privacy Rule: This rule sets national standards for the protection of PHI. It dictates how covered entities must use and disclose PHI, emphasizing the need for patient authorization for most uses and disclosures.
- Security Rule: This rule establishes national standards for protecting electronic PHI (ePHI) that is created, received, maintained, or transmitted by a covered entity. It requires administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of ePHI.
- Breach Notification Rule: This rule requires covered entities to notify affected individuals without unreasonable delay and no later than 60 days following the discovery of a breach of unsecured PHI.
- Business Associate Agreements (BAAs): If you engage with third-party vendors who handle PHI on your behalf (e.g., EHR systems, billing services), you must have a BAA in place that Artikels their responsibilities in protecting PHI.
“The Lord is a refuge for the oppressed, a stronghold in times of trouble.”
Psalm 9
9. In our practice, the patient’s privacy is a sanctuary we are called to protect.
Professional Liability Insurance
Even with the purest intentions and the highest level of skill, the possibility of unforeseen events or claims can arise. Professional liability insurance, often referred to as malpractice insurance, acts as a shield, offering financial protection against claims of negligence or errors in judgment related to the services you provide. It is a practical expression of foresight and responsibility, allowing you to practice with greater peace of mind, knowing you are protected should challenges emerge.Understanding the types of professional liability insurance is essential for adequate coverage:
- Claims-Made Policies: These policies provide coverage for claims that are made during the policy period, regardless of when the incident occurred. Coverage ceases if the policy is not renewed or is canceled.
- Occurrence Policies: These policies provide coverage for incidents that occur during the policy period, even if the claim is filed years later. They offer broader protection but are typically more expensive.
- Tail Coverage (or Extended Reporting Endorsement): This is an endorsement added to a claims-made policy that extends the reporting period for claims that may arise after the policy has expired or been canceled. It is crucial for protecting against future claims related to past services.
Developing Your Practice’s Business Plan

Embarking on the journey of establishing a functional medicine practice is a sacred calling, an invitation to serve humanity’s deepest need for holistic well-being. Just as a gardener meticulously plans the soil, sunlight, and seeds for a bountiful harvest, so too must you, as a spiritual steward of health, cultivate a robust business plan. This plan is not merely a document; it is a roadmap illuminated by divine intention, guiding your practice from inception to flourishing, ensuring it can touch countless lives with transformative care.This foundational step is where your vision takes tangible form.
It’s about translating your passion for functional medicine into a sustainable enterprise that can consistently offer healing and hope. A well-crafted business plan acts as your compass, helping you navigate the complexities of the marketplace with clarity and purpose, ensuring that your practice not only thrives financially but also fulfills its spiritual mandate to elevate human health.
Components of a Comprehensive Business Plan
A comprehensive business plan for a functional medicine clinic is a sacred blueprint, detailing every facet of your practice’s journey. It serves as a living document, a testament to your vision and a guide for your actions, ensuring that your practice is built on a foundation of foresight and spiritual integrity. Each section is a prayerful consideration of how you will manifest your healing gifts in the world.
- Executive Summary: This is the heart of your plan, a concise distillation of your practice’s mission, vision, services, and financial highlights. It’s a snapshot of the divine purpose driving your clinic.
- Company Description: Detail the core values, philosophy, and unique approach of your functional medicine practice. Emphasize your commitment to root-cause healing and patient empowerment.
- Services Offered: Clearly articulate the specific functional medicine services you will provide, such as personalized nutrition plans, gut health assessments, hormone balancing, and stress management protocols.
- Market Analysis: This section delves into understanding the landscape where your practice will bloom, identifying opportunities and understanding the needs of those you are called to serve.
- Organization and Management: Artikel the legal structure of your practice and the key personnel who will contribute to its spiritual and operational success.
- Marketing and Sales Strategy: Describe how you will lovingly connect with potential patients and guide them towards the healing journey your practice offers.
- Financial Projections: This is where you prayerfully estimate the financial resources needed and the potential for growth and sustainability.
- Funding Request (if applicable): If seeking external investment, clearly state your financial needs and how they will be utilized to expand your healing reach.
Market Analysis for a Functional Medicine Practice
The market analysis is a divine exploration of the terrain you are called to cultivate. It requires a deep understanding of the current health landscape, the unmet needs of individuals seeking true wellness, and the unique position your functional medicine practice will occupy. This discernment allows you to tailor your offerings to resonate with the deepest desires for healing and vitality.
- Industry Overview: Examine the growing demand for personalized, root-cause approaches to health, contrasting it with the limitations of conventional symptom-focused care. Highlight the increasing awareness of lifestyle and environmental factors in chronic disease.
- Target Market Identification: Define the specific groups of individuals who are most likely to benefit from and seek out your functional medicine services. Consider demographics, psychographics, and common health concerns.
- Needs Assessment: Understand the specific pain points, challenges, and aspirations of your target demographic. What are their frustrations with current healthcare? What are their dreams for vibrant health?
- Competitive Analysis: Identify other healthcare providers in your geographical area or online space who offer similar or complementary services. Understand their strengths, weaknesses, pricing, and patient experience. This is not about competition, but about understanding how you can uniquely serve.
- SWOT Analysis: A thoughtful examination of your practice’s Strengths, Weaknesses, Opportunities, and Threats. This allows for strategic planning to leverage your divine gifts and mitigate potential challenges.
Defining Your Target Patient Demographic and Their Needs
Identifying your ideal patient is akin to understanding the soil and climate best suited for a particular seed. It requires deep empathy and a spiritual attunement to the individuals who are most receptive to the transformative power of functional medicine. By understanding their unique journey, you can better serve their deepest needs.
When defining your target patient demographic, consider the following aspects, always with a heart of compassion and service:
- Demographics: Age, gender, income level, education, occupation, and geographical location. For instance, you might find that busy professionals aged 30-55 struggling with burnout and chronic fatigue are particularly drawn to your practice.
- Health Concerns: What are the most prevalent chronic conditions or health challenges your ideal patients face? This could include digestive issues, autoimmune diseases, hormonal imbalances, chronic pain, anxiety, or persistent fatigue.
- Values and Beliefs: What are their attitudes towards health and wellness? Are they proactive in seeking natural solutions? Do they value personalized care and a collaborative approach? Are they open to lifestyle changes?
- Lifestyle Factors: Consider their daily routines, stress levels, dietary habits, sleep patterns, and physical activity. Understanding these aspects helps in crafting truly personalized interventions.
- Patient Needs and Aspirations: Beyond specific conditions, what are their underlying desires? They likely seek not just symptom relief, but sustained energy, mental clarity, emotional balance, and the freedom to live a full, vibrant life. They yearn for a practitioner who truly listens and understands their unique story.
The greatest healing occurs when we meet patients precisely where they are, with understanding, grace, and a commitment to their unique journey of transformation.
Financial Projection Framework
The financial framework of your business plan is a prayerful stewardship of the resources entrusted to your practice. It requires careful consideration of both the initial investment and the ongoing streams of revenue, ensuring that your practice can sustainably serve those in need. This is about building a vessel strong enough to carry your healing mission.
A robust financial projection includes the following essential elements:
| Category | Description | Example Considerations |
|---|---|---|
| Startup Costs | The initial investment required to launch your practice. This is the seed capital needed to plant your healing garden. |
|
| Revenue Streams | The various ways your practice will generate income. These are the fruits of your dedicated service. |
|
| Operating Expenses | The ongoing costs associated with running your practice. These are the essential nutrients your practice needs to thrive. |
|
| Profitability Analysis | Forecasting your practice’s financial performance over a specific period (e.g., 1-5 years), including break-even analysis and projected profit margins. |
For example, a projection might estimate reaching profitability within 18-24 months, with a target profit margin of 15-20% after covering all expenses. This requires careful estimation of patient volume and average revenue per patient. |
Establishing Your Operational Framework

To truly embody the spirit of functional medicine, your practice’s operations must flow with grace and intention, mirroring the interconnectedness you teach your patients.
This framework is the vessel through which healing energy moves, ensuring every interaction, from the first whisper of inquiry to the sustained rhythm of ongoing care, is imbued with purpose and compassion. It is here, in the daily unfolding of your practice, that the seeds of transformation are sown and nurtured.The operational framework is more than just a set of procedures; it is the living, breathing embodiment of your practice’s values.
It’s about creating an environment where both patient and practitioner feel seen, heard, and supported, fostering a sacred space for healing to occur. By meticulously organizing the essential administrative processes and thoughtfully integrating technology, you build a foundation that allows the deeper work of functional medicine to flourish.
Patient Intake and Scheduling Processes
The journey of a patient into your care is the first sacred touchpoint, a moment pregnant with potential. Establishing a seamless and supportive intake process is paramount, setting the tone for their entire healing experience. This involves clearly defined steps that guide them from initial contact to their first appointment, ensuring they feel welcomed, informed, and empowered from the outset.
- Initial Inquiry and Welcome: Develop a clear protocol for responding to new patient inquiries, whether via phone, email, or a website contact form. This response should be prompt, empathetic, and provide essential information about your practice’s philosophy and services. Consider a brief welcome packet or email that introduces your approach to health and wellness.
- New Patient Paperwork: Design comprehensive yet manageable intake forms that capture a holistic view of the patient’s health history, lifestyle, and goals. This can include questionnaires on diet, sleep, stress, environmental exposures, and family history. Offer digital options for completion prior to the initial visit to save time and enhance convenience.
- Appointment Scheduling: Implement a user-friendly scheduling system that allows patients to book appointments easily, whether online or with the assistance of your administrative staff. Clearly communicate appointment availability, cancellation policies, and preparation instructions for their first visit.
- Pre-Appointment Preparation: Guide patients on how to best prepare for their initial consultation. This might include gathering previous lab results, a list of current medications and supplements, and a written account of their symptoms and concerns.
Technology Stack for a Modern Functional Medicine Practice
In today’s interconnected world, technology is not merely a tool but an extension of your healing intention, enabling efficient and effective patient care. A well-chosen technology stack acts as the nervous system of your practice, facilitating communication, streamlining workflows, and safeguarding precious patient information. It empowers you to focus on the heart of functional medicine: understanding the individual and guiding them toward optimal well-being.
The selection of your technology should be guided by a commitment to patient-centered care, security, and efficiency. Each component plays a vital role in creating a harmonious operational flow.
- Electronic Health Record (EHR) System: Choose an EHR system specifically designed or adaptable for functional medicine, capable of handling detailed patient histories, tracking progress, and integrating various types of data (labs, genetics, etc.). Examples of systems that can be adapted include systems like Practice Fusion (though always verify current features and suitability), or more specialized platforms that cater to integrative and functional medicine.
The key is a system that allows for deep dives into patient narratives and interconnected health factors.
- Billing and Practice Management Software: Select software that simplifies the complexities of billing, insurance claims, and patient payments. This could be integrated with your EHR or a standalone solution. Look for systems that can handle various payment models, including out-of-pocket services common in functional medicine.
- Secure Communication Tools: Implement secure patient portals for appointment scheduling, sharing lab results, messaging, and providing educational materials. This ensures privacy and HIPAA compliance while fostering ongoing engagement. Encrypted email services are also crucial for external communications.
- Telehealth Platform: A robust and user-friendly telehealth platform is essential for reaching patients remotely, offering flexibility and accessibility. Ensure it is secure, reliable, and integrates well with your other systems.
- Nutritional Analysis and Supplement Management Software: Tools that help track patient diets, provide personalized nutritional recommendations, and manage supplement protocols can significantly enhance care.
The Patient Experience: From Initial Contact to Ongoing Care
The patient experience is the sacred narrative of their journey with your practice, a tapestry woven with every interaction. From the very first moment they consider reaching out, to the deep, sustained engagement of ongoing care, each thread must be imbued with compassion, clarity, and a profound sense of partnership. This experience is not merely transactional; it is a transformative relationship built on trust and shared intention.
Cultivating an exceptional patient experience requires a conscious design of every touchpoint, ensuring that patients feel deeply understood, respected, and empowered throughout their healing journey.
- First Impression: The initial contact sets the stage. Whether through a warm phone call, an informative website, or a welcoming office environment, this first impression should convey professionalism, empathy, and a clear understanding of the patient’s potential needs.
- The Initial Consultation: This is a cornerstone of the functional medicine approach. It should be a comprehensive exploration, allowing ample time for the patient to share their story and for you to listen deeply. The goal is to create a safe space where the patient feels truly heard and understood, building a foundation of trust.
- Treatment Planning and Shared Decision-Making: Presenting a clear, personalized treatment plan that the patient understands and actively participates in creating is vital. This involves educating them about the rationale behind recommendations and empowering them to make informed choices about their health.
- Ongoing Support and Follow-Up: Regular check-ins, accessible communication channels, and consistent progress monitoring are crucial for sustained healing. This ongoing support reinforces the patient’s commitment and helps navigate challenges that may arise.
- Empowerment and Education: Throughout the process, continuously empower patients with knowledge about their bodies and their health. This fosters self-efficacy and encourages them to become active participants in their own well-being.
Patient Education and Engagement Strategy
Education is the light that illuminates the path to lasting wellness, and engagement is the vital spark that keeps the flame of healing burning bright. Your patient education and engagement strategy is the art of imparting wisdom, fostering understanding, and cultivating a deep, intrinsic motivation within each individual to embrace their health. It is about moving beyond passive reception to active participation in their own miraculous journey of restoration.
A well-crafted strategy ensures that patients are not just recipients of care, but active co-creators of their health, equipped with the knowledge and motivation to thrive.
- Personalized Educational Materials: Tailor educational content to each patient’s specific needs, conditions, and learning style. This can include curated articles, videos, infographics, and personalized handouts that explain their diagnosis, treatment plan, and the underlying principles of functional medicine.
- Workshops and Group Sessions: Offer group workshops on topics relevant to functional medicine, such as stress management, gut health, or mindful eating. These sessions foster a sense of community and provide a platform for shared learning and support.
- Online Resources and Patient Portal: Utilize your patient portal to host a library of educational resources, FAQs, and links to reputable external sources. This makes information readily accessible and encourages continuous learning.
- Behavior Change Support: Integrate strategies that support sustainable behavior change, such as motivational interviewing, goal setting, and accountability check-ins. This helps patients overcome obstacles and integrate new healthy habits into their lives.
- Feedback Mechanisms: Regularly solicit feedback from patients regarding their educational experience and engagement levels. This allows you to refine your strategies and ensure they are meeting the evolving needs of your patient population.
Crafting Your Service Offerings and Pricing

Embarking on the journey of a functional medicine practice is a sacred trust, an opportunity to guide souls toward vibrant health. As you shape the offerings and the value exchange, remember that your services are not merely transactions, but pathways to transformation. Let your pricing reflect the profound impact you aim to create, honoring both the dedication of your practice and the inherent worth of each individual seeking healing.The essence of functional medicine lies in its personalized approach, and your service structure should mirror this.
It’s about co-creating a journey, not simply dispensing a service. Consider how your offerings can empower patients, fostering a deep partnership in their pursuit of well-being. This section will illuminate the various avenues for structuring your services and establishing a pricing model that resonates with integrity and abundance.
Functional Medicine Service Delivery Models
The way you structure your services is a foundational element that shapes the patient experience and the sustainability of your practice. Each model offers a unique rhythm for engagement, catering to different needs and fostering varying levels of commitment. Understanding these models allows you to align your practice’s philosophy with its operational reality, creating a harmonious flow of care and value.
- Membership Models: These models foster a continuous, proactive relationship with patients. They often involve a recurring fee, granting access to a defined set of services, regular check-ins, and a proactive approach to health maintenance. This encourages ongoing engagement and allows for consistent support, aligning with the long-term nature of functional medicine. Examples include annual or monthly retainers that cover personalized consultations, lifestyle coaching, and access to educational resources.
- Package-Based Models: Packages offer a structured approach to addressing specific health concerns or achieving particular wellness goals. They bundle a defined set of assessments, consultations, and interventions over a set period. This provides clarity for patients regarding the scope of care and expected outcomes. Common packages might target areas like gut health restoration, hormonal balance, or energy optimization, typically spanning 3-6 months.
- Hybrid Models: Many practices find success by blending elements of both membership and package-based approaches. This allows for flexibility, offering a foundational membership for ongoing support while providing specialized packages for acute or specific health challenges. This can cater to a broader range of patient needs and financial considerations.
Common Functional Medicine Assessments and Testing Protocols
The diagnostic landscape of functional medicine is rich and detailed, aiming to uncover the root causes of imbalance. The assessments and tests you employ are your tools for deep inquiry, illuminating the intricate tapestry of a patient’s health. These investigations go beyond symptomatic treatment, seeking to understand the underlying physiological, biochemical, and environmental factors at play.The selection of assessments is a critical step in tailoring care.
It’s about asking the right questions of the body, guided by clinical expertise and a holistic understanding of human physiology. These tests provide the objective data that, when interpreted within the context of the individual’s story, form the bedrock of a personalized therapeutic plan.
- Biochemical and Nutritional Assessments: These often include comprehensive blood panels that go beyond standard markers, examining nutrient deficiencies, metabolic function, inflammation markers, and hormonal status. Examples include detailed vitamin and mineral panels, oxidative stress markers, and advanced lipid profiles.
- Gut Health Diagnostics: Understanding the microbiome is central to functional medicine. Tests like comprehensive stool analysis (CSA) evaluate the balance of beneficial and pathogenic bacteria, yeast, parasites, digestive enzyme function, and markers of inflammation in the gut.
- Hormonal Assessments: Salivary or urinary hormone testing provides a nuanced view of the body’s endocrine system, assessing levels of key hormones like cortisol, estrogen, progesterone, testosterone, and thyroid hormones throughout the day or cycle.
- Environmental and Toxicological Testing: These can include tests for heavy metals, mold exposure, and other environmental toxins that may be contributing to chronic health issues.
- Genetic Testing: While not always a primary diagnostic tool, genetic testing (e.g., SNPs analysis) can offer insights into an individual’s predispositions and how they may metabolize certain nutrients or respond to specific interventions.
Strategies for Transparent and Value-Based Pricing
Pricing in functional medicine is an art form that balances the immense value of restored health with the financial realities of patients and the sustainability of your practice. Transparency builds trust, and value-based pricing ensures that both parties feel honored in the exchange. It’s about communicating the profound return on investment that improved health provides.Your pricing should reflect the depth of expertise, the time invested in personalized care, and the comprehensive nature of the interventions.
It’s not merely the cost of a test or a consultation, but the pathway to reclaiming vitality and well-being that you are facilitating.
- Clear Service Bundling: Present your services in packages that clearly Artikel what is included, the duration of the program, and the expected outcomes. This provides a predictable framework for patients.
- Detailed Explanations of Value: Educate your patients on
-why* certain tests are recommended and how the information gained will directly inform their personalized plan. Emphasize the long-term benefits of addressing root causes, such as reduced future healthcare costs and improved quality of life. - Tiered Options: Consider offering different tiers of service within a package or membership model. This can accommodate varying budgets while still providing access to high-quality functional medicine care. For instance, a basic tier might include essential consultations and one core assessment, while a premium tier could add more advanced testing and additional coaching sessions.
- Focus on Outcomes: Frame your pricing around the desired health outcomes rather than just the individual services. For example, instead of pricing each consultation separately, price a “Gut Health Restoration Program” that includes a series of consultations and specific testing aimed at achieving a symptom-free digestive system.
- Payment Plans: Offering flexible payment options, such as installment plans, can make more comprehensive programs accessible to a wider range of individuals.
“The greatest wealth is health.”Virgil. Your pricing should reflect this profound truth, valuing the journey back to wholeness.
Direct-to-Patient Models Versus Insurance-Dependent Models
The financial framework of your practice is a significant choice, influencing accessibility, patient autonomy, and your ability to deliver care without compromise. Understanding the nuances of direct-to-patient versus insurance-dependent models is crucial for aligning your practice with your mission and values.Direct-to-patient, or out-of-pocket, models empower you to design your services based on optimal patient care rather than dictated by insurance formularies.
Insurance-dependent models, while potentially increasing accessibility for some, can introduce complexities and limitations.
- Direct-to-Patient (Out-of-Pocket) Model:
- Pros: Allows for complete freedom in designing service offerings and pricing. Fosters a direct relationship with patients, free from third-party payer restrictions. Can lead to higher profit margins and greater control over practice operations. Encourages patients to be more invested in their health journey as they are directly funding it.
- Cons: May limit accessibility for individuals with lower incomes or limited disposable income. Requires robust patient education to convey the value of services.
- Insurance-Dependent Model:
- Pros: Can make functional medicine services more accessible to a broader population, as insurance may cover a portion of the costs. Can attract a larger patient base who are accustomed to using insurance.
- Cons: Involves significant administrative overhead for billing, claims processing, and dealing with insurance company regulations. May necessitate limiting the scope of services or testing to what insurance deems “medically necessary.” Can lead to delays in payment and potential claim denials. The focus can sometimes shift from optimal patient care to what is reimbursable.
- Hybrid Model: Many practices operate on a hybrid model, accepting some insurance for specific services while maintaining an out-of-pocket structure for more comprehensive functional medicine assessments and personalized programs. This offers a balance, leveraging insurance where possible while retaining the autonomy of direct-to-patient care for core offerings.
Building Your Team and Culture

The journey of establishing a functional medicine practice is deeply intertwined with the souls who join you on this path. Your team is not merely a collection of individuals performing tasks; they are the embodiment of your practice’s spirit, the conduits through which healing energy flows to your patients. As you build this sacred space, invite into it those whose hearts resonate with the principles of holistic well-being and whose hands are guided by compassion.
This is about co-creation, about weaving a tapestry of shared purpose.As you gather your team, remember that each member is a vital thread in the fabric of your practice. Their unique gifts, when harmonized, create a symphony of care that uplifts and transforms. Cultivating a culture of shared vision, respect, and continuous growth is paramount. It is in this fertile ground that your practice will not only thrive but also serve as a beacon of hope and healing for all who seek it.
Key Roles and Responsibilities for Initial Practice Staff
To lay a strong foundation, it is essential to identify the core roles that will support the seamless operation of your functional medicine practice. These initial positions are designed to ensure that patient care is delivered with efficiency, empathy, and expertise. Each role plays a distinct yet interconnected part in the patient’s journey, from initial contact to ongoing support.
- Medical Assistant: This individual is crucial for direct patient support, including taking vital signs, preparing patients for examinations, assisting practitioners during procedures, and managing patient flow. They are often the first clinical point of contact and play a significant role in creating a comfortable and reassuring environment.
- Health Coach: A health coach is instrumental in empowering patients to make sustainable lifestyle changes. They work collaboratively with practitioners to translate complex health plans into actionable steps for patients, offering guidance, accountability, and motivational support. Their role is to help patients integrate functional medicine principles into their daily lives.
- Administrative Support: This role encompasses managing appointments, handling patient inquiries, processing payments, maintaining patient records, and ensuring the smooth day-to-day operations of the practice. This person is the gatekeeper of organization and the first point of contact for many, setting the tone for the patient experience.
Qualities and Skills for Functional Medicine Practitioners and Staff
When seeking individuals to join your practice, look beyond mere technical proficiency. The heart of functional medicine lies in its relational and holistic approach, and your team must reflect this ethos. Seek out those who possess a deep well of empathy, a genuine curiosity about the human body and spirit, and a commitment to lifelong learning.
- Empathy and Compassion: The ability to truly listen and connect with patients on an emotional level is non-negotiable. Look for individuals who demonstrate genuine care and understanding for the struggles and aspirations of others.
- Integrity and Ethical Conduct: Upholding the highest ethical standards is paramount in healthcare. Team members must be trustworthy, transparent, and committed to patient confidentiality and well-being.
- Curiosity and Continuous Learning: The field of functional medicine is constantly evolving. Seek individuals who possess an insatiable curiosity and a drive to expand their knowledge and skills, staying abreast of the latest research and therapeutic modalities.
- Collaborative Spirit: Functional medicine thrives on teamwork. Individuals should be adept at working harmoniously with others, valuing diverse perspectives, and contributing to a shared goal of patient optimal health.
- Problem-Solving Skills: The ability to think critically and creatively to address complex patient cases is essential. Team members should be able to analyze information, identify root causes, and develop effective strategies.
- Excellent Communication Skills: Clear, concise, and compassionate communication is vital, both with patients and among team members. This includes active listening and the ability to explain complex concepts in an understandable manner.
Fostering a Collaborative and Patient-Centered Team Culture
The culture of your practice is the invisible architecture that supports all your efforts. It is the shared energy and intention that permeates every interaction. To cultivate a truly collaborative and patient-centered environment, prioritize open communication, mutual respect, and a shared commitment to the patient’s journey toward wellness.
“The greatest gift you can give to others is the gift of your presence, fully attentive and truly caring.”
This principle should guide your team’s interactions. Encourage regular team meetings not just for operational updates but for sharing insights, celebrating successes, and collectively problem-solving patient cases. Create an atmosphere where every team member feels empowered to voice their ideas and concerns, knowing they will be heard and valued. Patient-centered care means that the patient’s needs, goals, and experiences are at the forefront of every decision and action.
This requires the team to operate as a unified front, with each member understanding their role in supporting the patient’s holistic well-being.
Training and Professional Development Needs for Your Team
The commitment to growth is a cornerstone of functional medicine. To ensure your team remains at the cutting edge of the field and continues to serve patients with excellence, invest in their ongoing training and professional development. This is not merely an expense; it is an investment in the very soul of your practice.
- Foundational Functional Medicine Training: Ensure all practitioners have completed rigorous training in functional medicine principles, diagnostics, and therapeutic approaches. This might include certifications from reputable organizations.
- Specialized Modality Training: Depending on your practice’s focus, offer training in specific areas such as gut health, hormone balance, detoxification, or advanced nutritional therapies.
- Health Coaching Certification and Ongoing Education: For health coaches, support their pursuit of recognized certifications and provide opportunities for them to deepen their understanding of behavioral change science and motivational interviewing.
- Communication and Interpersonal Skills Workshops: Regularly offer training in active listening, empathetic communication, conflict resolution, and cultural competency to enhance patient interactions and team dynamics.
- Technology and Software Training: As you implement new practice management software, electronic health records, or diagnostic tools, ensure comprehensive training for all relevant staff members.
- Mind-Body Connection and Stress Management Techniques: Equip your team with an understanding of the mind-body connection and provide them with tools and techniques for managing their own stress, enabling them to better guide patients.
- Business and Practice Management Skills: For administrative and leadership roles, offer training in areas such as customer service, financial management, and effective practice operations.
Marketing and Patient Acquisition Strategies

Embarking on the journey to establish a functional medicine practice is a sacred calling, a commitment to guiding souls toward holistic well-being. Yet, even the most profound healing modalities require connection. This chapter illuminates the art and science of reaching those who seek your unique gifts, weaving a tapestry of intention and outreach that honors both your practice and the individuals you are destined to serve.
Remember, marketing in this realm is not about selling, but about illuminating the path to vibrant health.The spirit of functional medicine thrives on education and empowerment. Therefore, our marketing endeavors must mirror this ethos, offering genuine value and fostering trust. We are not merely attracting patients; we are cultivating a community of seekers who resonate with our vision of wellness.
This approach ensures that those who find you are aligned with your philosophy, creating a foundation for deep and lasting healing partnerships.
Creating a Content Marketing Plan to Attract Potential Patients
A well-crafted content marketing plan acts as a beacon, drawing in those who are searching for answers and solutions that align with the functional medicine paradigm. It is about sharing wisdom, demystifying complex health concepts, and demonstrating the transformative power of an individualized, root-cause approach. This plan should be guided by compassion and a genuine desire to educate, empowering potential patients to take an active role in their healing journey.The essence of effective content marketing lies in understanding the unmet needs and questions of your ideal patient.
By addressing these directly and offering insightful, evidence-based information, you build credibility and establish yourself as a trusted authority. This is not a fleeting endeavor but a continuous practice of sharing your light, nurturing curiosity, and guiding individuals toward the possibility of profound health.Consider a content calendar that balances various forms of educational outreach:
- Blog Posts: Delve into specific conditions (e.g., “Understanding the Gut-Brain Axis in Anxiety,” “The Role of Inflammation in Autoimmune Disease”), explore foundational principles of functional medicine (e.g., “The Pillars of Vibrant Health,” “Why Diet is Just One Piece of the Puzzle”), or share inspiring patient success stories (with appropriate anonymization and consent).
- Ebooks and Guides: Offer downloadable resources that provide in-depth knowledge on key topics, such as “A Beginner’s Guide to Detoxification” or “Navigating Hormonal Imbalances Naturally.” These serve as valuable lead magnets.
- Webinars and Online Workshops: Host live or recorded sessions on trending health topics or core functional medicine concepts. This allows for direct interaction and Q&A, fostering a deeper connection.
- Infographics and Visual Content: Translate complex information into easily digestible visuals that can be shared across social media platforms. For example, an infographic illustrating the interconnectedness of the body’s systems or the stages of chronic disease.
- Podcasts: Share your expertise and host conversations with other practitioners or inspiring individuals in the wellness space. This medium allows for a more intimate and personal connection with your audience.
The creation of this content should be infused with authenticity, reflecting your unique voice and the compassionate spirit of your practice. Each piece of content is an opportunity to plant seeds of hope and inspire a journey toward healing.
Effective Online Presence Strategies Including Website and Social Media
Your online presence is the digital embodiment of your practice’s spirit and mission. It is the first encounter many will have with your healing sanctuary, and as such, it must be a reflection of the care, expertise, and profound potential for transformation that you offer. This digital footprint should be meticulously cultivated to be both informative and inviting, guiding individuals towards the understanding and support they seek.Your website is the cornerstone of your online presence, serving as a virtual reception and educational hub.
It should be designed with intention, reflecting the calm, organized, and holistic nature of your practice. Beyond aesthetics, it must be a functional tool that clearly communicates your philosophy, services, and the unique benefits of functional medicine.Key elements for an impactful website include:
- Clear Mission and Philosophy Statement: Articulate your core beliefs and the guiding principles of your practice. This helps potential patients understand if your approach resonates with their needs.
- Detailed Service Descriptions: Clearly Artikel the conditions you address, the diagnostic tools you employ, and the therapeutic modalities you utilize. Explain the
-why* behind your approach, emphasizing root-cause resolution. - Practitioner Bios: Share the journey and expertise of your practitioners, highlighting their passion for functional medicine and their commitment to patient well-being.
- Testimonials and Success Stories: With explicit consent and anonymization, showcase the positive outcomes and transformations experienced by your patients. This builds trust and offers tangible proof of your practice’s efficacy.
- Educational Resources: Integrate your blog, downloadable guides, and links to webinars. This positions you as a valuable source of information and empowers visitors.
- Easy Contact and Appointment Booking: Streamline the process for potential patients to connect with your practice and schedule initial consultations.
- Mobile Responsiveness and Fast Loading Speed: Ensure your website is accessible and user-friendly across all devices, reflecting a modern and efficient practice.
Social media, when approached with mindfulness and integrity, can amplify your message and foster a vibrant community. It is a space for connection, education, and inspiration, allowing you to share your wisdom in real-time and engage with a broader audience.When utilizing social media platforms, consider the following:
- Platform Selection: Choose platforms that align with your target audience. For functional medicine, platforms like Instagram (visuals, short tips), Facebook (community building, longer posts, events), LinkedIn (professional networking, practice insights), and even YouTube (educational videos, Q&A sessions) can be highly effective.
- Consistent Posting Schedule: Maintain a regular rhythm of sharing valuable content, whether it’s daily tips, weekly blog highlights, or monthly Q&A sessions.
- Engaging Content: Go beyond simply posting links. Share personal insights, behind-the-scenes glimpses of your practice (while respecting patient privacy), and ask questions to encourage interaction.
- Visual Appeal: Use high-quality images and videos that reflect the natural, holistic, and vibrant aspects of wellness.
- Community Engagement: Respond to comments and messages promptly and thoughtfully. Foster a sense of belonging and support within your online community.
- Ethical Sharing: Always prioritize patient privacy and confidentiality. Avoid sharing any identifiable patient information without explicit, written consent.
“Your online presence is not just a website; it is a digital temple of healing, inviting souls to discover their path to vibrant life.”
Methods for Building Referral Relationships with Other Healthcare Providers
The spirit of functional medicine thrives in collaboration. Building strong referral relationships with other healthcare providers is not merely a strategic business move; it is a sacred alliance that expands the reach of holistic care and ensures patients receive comprehensive support. These partnerships are founded on mutual respect, shared values, and a deep understanding of how each practitioner contributes to the patient’s overall well-being.When approaching other healthcare professionals, remember that you are extending an invitation to co-create healing.
Your aim is to educate them about the unique value of functional medicine and how it can complement their existing approaches, thereby enhancing patient outcomes. This requires clear communication, demonstrable expertise, and a genuine commitment to the patient’s best interests.Effective strategies for cultivating these vital connections include:
- Educate and Inform: Schedule brief meetings or lunches with physicians, chiropractors, acupuncturists, nutritionists, therapists, and other allied health professionals. Share concise information about functional medicine principles, the types of conditions you effectively address, and the diagnostic and therapeutic modalities you utilize. Provide them with brochures or one-page summaries that clearly Artikel your services and philosophy.
- Highlight Complementary Approaches: Emphasize how functional medicine can work in synergy with conventional medicine. For instance, explaining how you can help patients optimize their health and reduce medication reliance for chronic conditions, or how you can support patients undergoing conventional treatments by addressing underlying imbalances.
- Offer Value-Added Services: Consider offering to provide educational workshops or presentations to the staff of referring practices on topics relevant to functional medicine. This demonstrates your expertise and fosters goodwill.
- Establish Clear Communication Protocols: Develop a system for timely and thorough communication regarding shared patients. This includes providing detailed reports of your findings and treatment plans, and being receptive to feedback from referring providers. A secure, HIPAA-compliant portal for sharing patient information can be invaluable.
- Showcase Success Stories: When appropriate and with patient consent, share anonymized case studies that illustrate the positive impact of your collaborative efforts. This provides tangible evidence of the benefits of referring patients to your practice.
- Attend Professional Networking Events: Participate in local medical and wellness conferences, seminars, and community health events. These provide opportunities to meet and connect with potential referral partners in a less formal setting.
- Be a Reliable and Responsive Partner: Consistently provide high-quality care to referred patients and ensure prompt communication. A strong reputation for excellence and collaboration will naturally lead to increased referrals.
“True healing is a symphony, where each practitioner plays their unique instrument in harmony to create a masterpiece of well-being for the patient.”
Ethical Considerations in Marketing Functional Medicine Services
The practice of functional medicine is rooted in integrity, compassion, and a profound respect for the individual’s healing journey. When we extend this ethos into our marketing efforts, we must navigate with unwavering ethical consciousness. Our communication should always be truthful, transparent, and focused on empowering individuals, rather than exploiting their vulnerabilities or making unsubstantiated claims.In the realm of functional medicine, ethical marketing means fostering an environment of informed consent and realistic expectations.
We are offering a path to wellness, not a guaranteed cure, and our messaging must reflect this nuanced reality. Transparency about our methodologies, pricing, and the expected outcomes is paramount to building enduring trust.Key ethical considerations include:
- Truthful and Accurate Representation: All marketing materials must accurately reflect the services offered, the qualifications of practitioners, and the scientific basis for the functional medicine approach. Avoid hyperbole or making definitive promises of cures.
- Avoiding Exploitative Language: Refrain from preying on fear, desperation, or misinformation. Marketing should inspire hope and offer solutions, not exploit anxieties about illness.
- Transparency in Pricing and Services: Clearly communicate all costs associated with consultations, testing, and treatments. Avoid hidden fees or misleading pricing structures. Explain the value proposition of your services in a clear and understandable manner.
- Respect for Patient Confidentiality: Never share patient testimonials or case studies without explicit, written consent. Ensure all identifying information is removed or anonymized.
- Managing Expectations: While functional medicine can achieve remarkable results, it is essential to set realistic expectations. Clearly communicate that healing is a process, and outcomes can vary. Avoid language that suggests guaranteed results or rapid fixes.
- Scope of Practice: Ensure that your marketing efforts do not overstep the boundaries of your professional scope of practice or make claims that cannot be substantiated by your training and expertise.
- Evidence-Based Claims: Whenever possible, support claims made in marketing materials with scientific evidence or reputable research. If making claims about specific outcomes, be prepared to provide supporting data.
- Avoiding Unfair Comparisons: Do not disparage other healthcare modalities or practitioners. Focus on the unique benefits of functional medicine without undermining the value of other approaches.
By adhering to these ethical principles, we not only safeguard the integrity of our practice but also cultivate a deeper, more authentic connection with those who seek our guidance, ensuring that our outreach is a true reflection of our commitment to holistic well-being.
Implementing Patient Care Protocols

Embarking on the journey of a functional medicine practice is akin to tending a sacred garden. It requires diligent preparation, deep understanding, and a commitment to nurturing growth. Just as a gardener designs a planting schedule and monitors soil health, a functional medicine practitioner must establish robust protocols to guide the patient’s healing path, ensuring each step is taken with intention and wisdom.
These protocols are not rigid rules, but rather a compassionate framework that honors the unique spirit and journey of every individual.The essence of functional medicine lies in its personalized approach, recognizing that true wellness blossoms when we address the root causes of imbalance. Implementing patient care protocols is the art of translating this philosophy into tangible, effective action. It is about creating a sacred space where the patient feels seen, heard, and empowered to reclaim their vitality.
Designing Initial Patient Consultations and History Taking, How to start a functional medicine practice
The initial consultation is the fertile ground where understanding takes root. It’s an opportunity to create a safe haven for the patient to share their story, their struggles, and their deepest aspirations for health. This sacred exchange goes beyond listing symptoms; it delves into the tapestry of their life, seeking to understand the intricate connections between their physical, emotional, and spiritual well-being.
A comprehensive history-taking process honors the whole person, recognizing that their health journey is woven with unique threads of experience.A structured yet flexible approach to history taking ensures no vital thread is missed. This often involves:
- Intake Forms: Detailed questionnaires covering medical history, family history, lifestyle habits (diet, sleep, exercise, stress), environmental exposures, and emotional well-being. These forms act as a preliminary map, highlighting areas for deeper exploration.
- In-Depth Interview: A one-on-one conversation, guided by empathy and active listening, allowing the patient to elaborate on their journey. This is where the practitioner can discern patterns, uncover hidden stressors, and understand the patient’s unique perception of their health.
- Timeline Creation: Collaboratively mapping out significant life events and health changes over time can reveal crucial insights into the genesis of their current imbalances.
- Review of Previous Labs and Records: Understanding past medical interventions and diagnostic findings provides a historical context for the current situation.
Developing Personalized Functional Medicine Treatment Plans
Once the deep understanding from the initial consultation is established, the sacred work of crafting a personalized treatment plan begins. This plan is not a one-size-fits-all prescription, but a divinely inspired blueprint, co-created with the patient, designed to restore harmony and vitality from the inside out. It acknowledges that each soul’s journey is unique, and therefore, their path to wellness must be equally distinct.The development of these plans involves a holistic consideration of multiple dimensions:
- Root Cause Analysis: Identifying the underlying biochemical, physiological, and environmental factors contributing to the patient’s symptoms. This moves beyond symptom management to address the core imbalances.
- Integration of Modalities: Combining various evidence-based interventions, tailored to the individual’s needs and preferences. This might include nutritional therapy, targeted supplementation, detoxification protocols, stress management techniques, sleep optimization, and movement therapies.
- Patient Empowerment: Ensuring the patient is an active participant in their healing journey. This involves clear education, setting realistic expectations, and fostering a sense of agency and responsibility.
- Phased Approach: Often, treatment plans are implemented in phases, starting with foundational support and gradually progressing to more targeted interventions as the patient’s body responds and strengthens.
“The body is a sacred vessel, capable of profound healing when given the right conditions.”
Methods for Monitoring Patient Progress and Adjusting Protocols
The journey of healing is a dynamic dance, requiring constant attunement and gentle adjustments. Monitoring patient progress is not merely about tracking symptom changes, but about observing the subtle shifts in their energy, their spirit, and their overall sense of well-being. This continuous feedback loop allows for the graceful adaptation of protocols, ensuring they remain aligned with the patient’s evolving needs.Effective monitoring involves a multi-faceted approach:
- Regular Follow-Up Appointments: Scheduled check-ins, both in-person and virtual, to discuss progress, address challenges, and celebrate victories. These appointments are sacred opportunities for continued dialogue and support.
- Symptom Tracking and Journals: Encouraging patients to keep detailed records of their symptoms, energy levels, mood, and responses to interventions. This provides invaluable real-time data.
- Biomarker Re-evaluation: Periodically re-testing relevant laboratory markers to objectively assess physiological changes and the effectiveness of interventions. This provides scientific validation for the healing process.
- Subjective Feedback: Actively soliciting the patient’s perception of their well-being, including their energy, sleep quality, mood, and overall life satisfaction. Their lived experience is a crucial indicator of progress.
- Protocol Adjustment: Based on the gathered data and patient feedback, making informed and compassionate adjustments to the treatment plan. This might involve modifying dosages, changing interventions, or introducing new strategies.
Strategies for Integrating Lifestyle Interventions into Care
Lifestyle interventions are the bedrock of true, sustainable wellness. They are the daily practices that nourish the body, calm the mind, and uplift the spirit. Integrating these profound practices into a functional medicine protocol is about weaving them into the fabric of the patient’s life, making them not a burden, but a source of joy and vitality. These are the seeds of transformation that, when nurtured, yield abundant harvests of health.Key lifestyle interventions to integrate include:
- Nutritional Guidance: Educating patients on the principles of nutrient-dense, whole-foods-based diets that support their specific needs. This involves understanding food sensitivities, optimizing macronutrient balance, and addressing micronutrient deficiencies.
- Sleep Optimization: Guiding patients to establish healthy sleep hygiene practices, addressing factors that disrupt sleep, and creating a restorative sleep environment. Quality sleep is a fundamental pillar of healing.
- Stress Management Techniques: Introducing practices such as mindfulness, meditation, deep breathing exercises, yoga, and time in nature to help regulate the nervous system and reduce the impact of chronic stress.
- Mindful Movement: Encouraging regular physical activity that is enjoyable and sustainable for the individual, promoting cardiovascular health, strength, and flexibility.
- Environmental Awareness: Educating patients about potential environmental toxins and guiding them in making conscious choices to minimize exposure and support their body’s detoxification pathways.
- Social Connection and Purpose: Recognizing the profound impact of supportive relationships and a sense of purpose on overall well-being, and encouraging patients to cultivate these aspects of their lives.
Financial Management and Billing

As you embark on the sacred journey of building a functional medicine practice, remember that stewarding its resources is as vital as nurturing the health of your patients. True abundance flows not just from outward success, but from inner order and wise stewardship. This section is dedicated to cultivating that inner order, ensuring your practice’s financial health mirrors the vitality you bring to your clients.
It’s about transforming the often-feared realm of numbers into a sacred space of clarity, integrity, and purposeful growth.Financial management and billing are the arteries through which the lifeblood of your practice flows. By establishing robust systems, you honor the value of your work, ensure sustainability, and create a foundation of trust with both your team and your patients. This is not merely about accounting; it is about aligning your financial practices with your core mission of healing and service.
Practice Finance and Bookkeeping Systems
A well-organized financial system is the bedrock of a thriving practice. It allows for clear oversight, informed decision-making, and the peace of mind that comes from knowing your practice is operating with integrity and efficiency. Think of it as creating a sacred ledger, where every transaction is recorded with reverence for its contribution to your mission.
“The greatest wealth is to live content with little.” – Plato
Establishing a system for managing practice finances and bookkeeping involves several key elements:
- Choosing Accounting Software: Select user-friendly accounting software designed for small businesses or medical practices. Popular options include QuickBooks, Xero, or specialized medical practice management software. These tools automate many tasks, reduce errors, and provide real-time financial insights.
- Chart of Accounts: Develop a comprehensive chart of accounts tailored to your practice. This categorizes all income and expenses, such as patient revenue, lab fees, supplement sales, rent, salaries, and marketing costs. A well-structured chart of accounts is crucial for accurate reporting.
- Bookkeeping Procedures: Implement consistent daily, weekly, and monthly bookkeeping procedures. This includes recording all transactions, reconciling bank statements, tracking petty cash, and managing invoices. Consistency is key to maintaining accurate financial records.
- Expense Tracking: Meticulously track all business expenses. Categorize them appropriately for tax purposes and to understand where your practice’s resources are being allocated. This diligence ensures you maximize deductions and identify areas for potential cost savings.
- Budgeting and Forecasting: Create an annual budget that projects income and expenses. Regularly review your budget against actual performance and adjust your forecasts as needed. This proactive approach helps you anticipate financial needs and opportunities.
Medical Billing and Coding for Functional Medicine Services
The process of medical billing and coding in functional medicine requires a nuanced approach, acknowledging the unique nature of these services. It’s about accurately translating the comprehensive care you provide into a language that insurers and patients understand, ensuring fair compensation and transparent communication. This is an act of clarity, ensuring the value of your holistic approach is recognized.
“Clarity is the first step to transformation.” – Unknown
Detailing the process of medical billing and coding for functional medicine services involves:
- Understanding CPT and ICD-10 Codes: Familiarize yourself with relevant Current Procedural Terminology (CPT) codes for evaluation and management, and International Classification of Diseases, 10th Revision (ICD-10) codes for diagnoses. Functional medicine often requires more detailed diagnostic coding to capture the complexity of patient conditions.
- Naturopathic/Holistic Billing: Many functional medicine practices operate outside of traditional insurance models or offer services not fully covered by standard plans. This may involve a blend of insurance billing for specific covered services and direct patient payment for others.
- Superbills and Patient Statements: Generate clear and detailed superbills or patient statements that accurately reflect services rendered, dates of service, and costs. These documents are essential for patient reimbursement and for their own record-keeping.
- Working with Billing Specialists: Consider partnering with a medical billing service that has experience with functional medicine or holistic practices. They can navigate the complexities of insurance claims, denials, and appeals, freeing up your time to focus on patient care.
- Insurance Verification: Before providing services, always verify patient insurance benefits to understand coverage for specific functional medicine modalities. This proactive step helps manage patient expectations regarding out-of-pocket costs.
Managing Accounts Receivable and Patient Payments
The timely collection of payments is crucial for the financial stability of your practice. Implementing clear, compassionate, and efficient systems for managing accounts receivable and patient payments ensures a healthy cash flow and maintains positive patient relationships. This is about honoring the exchange of value with grace and professionalism.
“Cash flow is king.” – Unknown
Strategies for managing accounts receivable and patient payments include:
- Clear Payment Policies: Establish and clearly communicate your practice’s payment policies to patients at the outset of their care. This includes information on co-pays, deductibles, payment plans, and accepted forms of payment.
- Upfront Payment Collection: For non-covered services or for patients without insurance, collect payment at the time of service. This significantly reduces the burden of accounts receivable.
- Payment Plans and Financing: Offer flexible payment plans or partner with third-party financing options for patients who need assistance with larger treatment costs. This makes your services more accessible.
- Automated Reminders: Utilize your practice management software to send automated payment reminders via email or text message for outstanding balances.
- Follow-up Procedures: Develop a systematic process for following up on overdue accounts. This might involve phone calls, reminder letters, and, as a last resort, engaging a collection agency. Ensure all follow-up is conducted with professionalism and respect.
- Patient Portal for Payments: Implement a secure online patient portal where patients can view their statements, make payments, and manage their account information. This offers convenience and efficiency.
Financial Reporting and Analysis
Regularly reviewing your practice’s financial reports is like consulting a spiritual compass, guiding you towards sustainable growth and aligning your actions with your deepest intentions. This process provides invaluable insights into the health of your practice, allowing you to make informed decisions and ensure your resources are being used in the most effective way.
“What gets measured, gets managed.”
Peter Drucker
Best practices for financial reporting and analysis include:
- Key Financial Statements: Regularly generate and review essential financial statements, including the Profit and Loss (P&L) statement, Balance Sheet, and Cash Flow Statement. Understanding these documents is fundamental to financial stewardship.
- Key Performance Indicators (KPIs): Identify and track key performance indicators relevant to your practice. These might include:
- Revenue per patient
- Patient retention rate
- Average visit revenue
- Accounts receivable aging
- Overhead percentage
- Profit margin
- Regular Review Meetings: Schedule dedicated time, at least monthly, to review your financial reports and KPIs. If you have a team, involve them in these discussions to foster a shared understanding of the practice’s financial health.
- Trend Analysis: Analyze financial data over time to identify trends, patterns, and potential areas for improvement or concern. This historical perspective is invaluable for forecasting and strategic planning.
- Benchmarking: Where possible, compare your practice’s financial performance against industry benchmarks to identify areas where you are excelling or where there is room for growth.
- Budget vs. Actual Analysis: Compare your actual financial performance against your budget. Understand the variances and develop strategies to address any significant deviations.
Continuous Improvement and Growth
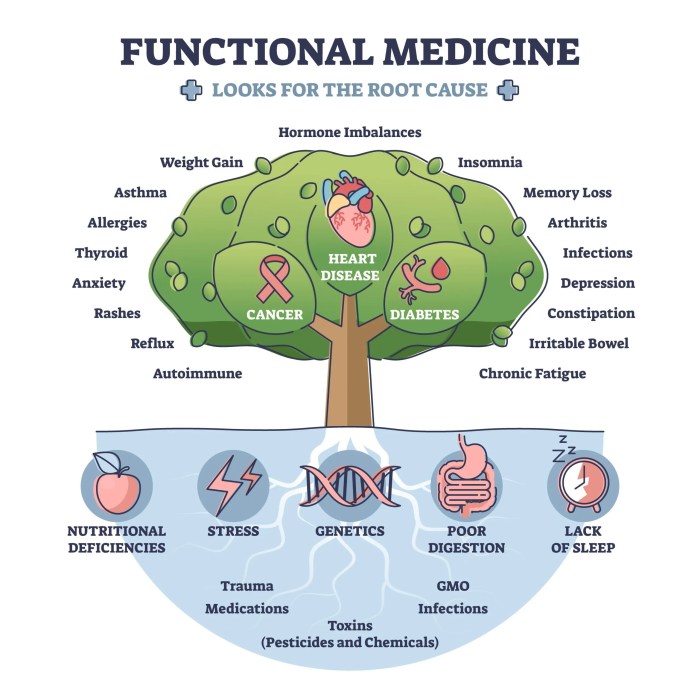
The journey of establishing a functional medicine practice is not a destination but a sacred unfolding. As you nurture this vital space for healing, embracing a spirit of continuous improvement and growth becomes paramount. This ongoing evolution is akin to tending a garden; it requires diligent observation, thoughtful adaptation, and a deep commitment to flourishing, not just for your practice, but for the lives you touch.This commitment to perpetual learning and refinement is the bedrock of enduring excellence.
Ngasal mau buka praktik kedokteran fungsional? Kudu ngerti dulu seluk beluknya, kayak gimana sih how to become a holistic medicine practitioner biar makin komprehensif. Abis itu, baru deh mikirin step by step buat bangun praktik fungsional yang mantap.
It ensures that your practice remains a beacon of innovative, patient-centered care, adapting to the ever-evolving landscape of health and well-being. By actively seeking to understand what works best and how to serve more profoundly, you honor the trust placed in you and amplify your capacity to make a transformative difference.
Practice Performance and Patient Outcome Metrics
To truly understand the pulse of your practice and the depth of its healing impact, we must establish clear indicators of progress. These metrics serve as our spiritual compass, guiding us toward greater effectiveness and illuminating the path of transformation for each soul that enters your care. They are not merely numbers, but reflections of the well-being you are fostering.Key performance indicators provide a vital lens through which to view the health and vitality of your practice.
They offer tangible evidence of your efforts and highlight areas where your spiritual intention can be further amplified.
- Patient Retention Rate: This metric reflects the enduring trust and satisfaction of your patients. A high retention rate signifies that patients feel deeply understood, supported, and are experiencing sustained positive outcomes. It is a testament to the sacred connection you are building.
- Patient Outcome Scores: Utilizing validated questionnaires and assessments (e.g., symptom burden scales, quality of life indices, functional assessments) before and after interventions provides quantifiable evidence of patient progress. These scores speak to the restoration of vitality and the return of joy to their lives.
- Appointment Adherence: The consistency with which patients attend their scheduled appointments is a powerful indicator of their engagement and belief in the healing process. It signifies their commitment to their own well-being.
- Referral Rate: When patients feel profoundly cared for and experience genuine transformation, they naturally become advocates. A strong referral rate is a spiritual echo of the positive impact your practice is having on the community.
- Wait Times: While seemingly operational, excessively long wait times can be a subtle barrier to care and indicate strain within the system. Optimizing this flow ensures that patients can access healing when they are most receptive.
- Staff Satisfaction: A harmonious and inspired team is crucial for creating a nurturing environment. Measuring staff morale and satisfaction ensures that the collective energy of your practice is vibrant and supportive.
Patient Feedback Gathering and Action
The whispers of your patients’ experiences are sacred messages, offering invaluable insights into the heart of your practice. Gathering this feedback with an open spirit and acting upon it with wisdom is a profound act of service, ensuring that your practice remains attuned to the deepest needs of those you serve.Engaging with patient feedback is a continuous dialogue, a sacred exchange that allows for the refinement of your healing ministry.
It is through listening deeply that we can best serve.
- Anonymous Surveys: Implement regular, anonymous surveys using online platforms or simple paper forms at the end of appointments. These provide a safe space for patients to share their honest reflections without reservation. Focus questions on clarity of explanations, perceived empathy, effectiveness of treatment, and overall experience.
- Post-Visit Follow-Ups: A brief phone call or personalized email a few days after an appointment can offer an opportunity for patients to share immediate impressions or address any lingering questions. This demonstrates a continued commitment to their well-being.
- Patient Advisory Council: For established practices, consider forming a small council of engaged patients who can offer deeper, more nuanced feedback on services, communication, and overall practice direction. This cultivates a sense of shared purpose.
- Open Communication Channels: Ensure that patients know how to reach out with concerns or suggestions at any time, whether through a dedicated email address or a designated point person within the practice.
- Regular Review Meetings: Dedicate time in team meetings to collectively review feedback received. Discuss common themes, identify areas for improvement, and brainstorm actionable strategies. This fosters a shared responsibility for growth.
- Closing the Loop: When specific feedback leads to a change, communicate this back to your patients. For example, if multiple patients requested easier online booking, announce when this feature is implemented. This shows that their voices are heard and valued.
Staying Current with Functional Medicine Research and Advancements
The field of functional medicine is a vibrant, ever-expanding universe of knowledge. To remain a true guide in this space, a commitment to continuous learning and integration of new discoveries is essential. This dedication ensures that your practice remains at the forefront of innovative healing, offering the most profound and effective care possible.The pursuit of knowledge in functional medicine is a spiritual discipline, a commitment to understanding the intricate tapestry of the human body and its innate capacity for healing.
- Professional Journals and Publications: Regularly subscribe to and review leading peer-reviewed journals in areas such as epigenetics, microbiome research, environmental medicine, and personalized nutrition. Examples include the
-American Journal of Clinical Nutrition*,
-Cell Metabolism*, and
-Nature Medicine*. - Conferences and Workshops: Actively participate in national and international functional medicine conferences (e.g., those hosted by the Institute for Functional Medicine (IFM), American Academy of Anti-Aging Medicine (A4M)). These events offer invaluable insights from leading researchers and clinicians.
- Online Learning Platforms and Webinars: Many reputable organizations offer online courses, webinars, and certifications that delve into specific areas of functional medicine. This allows for flexible, ongoing education.
- Networking with Peers: Engage in regular dialogue with other functional medicine practitioners. Sharing experiences, case studies, and insights fosters a collective wisdom that transcends individual learning.
- Research Review Groups: Consider forming or joining a small group of practitioners dedicated to critically reviewing and discussing new research findings. This collaborative approach enhances understanding and application.
- Following Key Researchers and Innovators: Stay informed about the work of leading scientists and clinicians in the field through their publications, social media, and speaking engagements.
Practice Expansion and Diversification Opportunities
As your practice flourishes and your capacity to serve deepens, the natural next step is to explore avenues for expansion and diversification. This is not about mere growth, but about extending your healing reach and offering a more comprehensive spectrum of well-being services, thereby touching more lives and fulfilling your practice’s sacred mission.The spirit of expansion is about recognizing the interconnectedness of well-being and offering a holistic approach that nurtures every facet of a person’s journey toward vitality.
- Adding New Services: Introduce complementary services that align with your core functional medicine philosophy. This could include:
- Nutritional counseling and meal planning services.
- Mind-body therapies such as meditation, yoga, or stress management coaching.
- Detoxification and cleansing programs.
- Specialized testing interpretation (e.g., advanced genetic, hormone, or gut microbiome analysis).
- Integrative physical therapy or movement assessment.
- Developing Group Programs: Create group programs focused on specific health concerns or wellness goals. Examples include:
- Weight management and metabolic health workshops.
- Stress reduction and resilience building courses.
- Gut health optimization seminars.
- Sleep hygiene and improvement programs.
Group formats can be highly cost-effective and foster a powerful sense of community and shared healing.
- Telehealth Expansion: Leverage technology to extend your reach beyond geographical limitations. Offering virtual consultations and follow-ups allows you to serve a broader patient base and provide greater convenience.
- Partnerships and Collaborations: Forge alliances with other wellness professionals or complementary healthcare providers. This could involve co-hosting events, cross-referring patients, or developing integrated care pathways. Think about partnering with local gyms, mindfulness centers, or specialized labs.
- Product Development: Consider developing or curating high-quality, evidence-based wellness products that complement your services. This might include custom-formulated supplements, educational materials, or wellness kits. Ensure any products align strictly with your ethical and scientific standards.
- Establishing Satellite Clinics or Outreach Programs: If demand warrants, explore the possibility of opening satellite locations in underserved areas or developing outreach programs within communities to increase accessibility to functional medicine care.
Last Recap: How To Start A Functional Medicine Practice

Embarking on the path to establish a functional medicine practice is a multifaceted endeavor, yet one that promises profound rewards. By understanding the core principles, meticulously laying the legal and business foundations, and focusing on patient-centered care, you can create a practice that truly makes a difference. This comprehensive guide has provided the essential framework, from operational details to marketing and financial management, empowering you to build a successful and impactful functional medicine clinic.
Embrace the opportunity to transform lives through this innovative healthcare model.
Answers to Common Questions
What are the typical startup costs for a functional medicine practice?
Startup costs can vary significantly but generally include expenses for office space, equipment (e.g., diagnostic tools), technology (EHR, billing software), initial marketing, legal fees, licenses, insurance, and initial staffing. A detailed financial projection within your business plan is crucial for estimating these costs.
How do I differentiate my functional medicine practice from others?
Differentiation can be achieved by specializing in a particular niche (e.g., gut health, autoimmune conditions), developing unique patient programs, offering exceptional patient experience, building strong referral networks, and clearly articulating your practice’s philosophy and unique value proposition in your marketing.
What are the ongoing challenges in running a functional medicine practice?
Ongoing challenges often include patient adherence to treatment plans, managing complex patient cases, staying updated with rapidly evolving research, navigating insurance complexities (if applicable), maintaining financial viability, and effectively marketing to attract and retain patients.
How important is patient education in a functional medicine setting?
Patient education is paramount in functional medicine. It empowers patients to understand their health conditions, the rationale behind treatment plans, and the importance of lifestyle modifications. Effective education fosters engagement, improves adherence, and ultimately leads to better long-term outcomes.
What kind of technology is essential for a functional medicine practice?
Essential technology includes a robust Electronic Health Record (EHR) system, secure patient communication platforms, reliable billing and practice management software, and potentially specialized diagnostic software or patient portals for accessing test results and educational materials.




